Birth Trauma: A Story of Survival, Vulnerability & Healing
When a friend, Lauren, shared this with me, it captured the profound disorientation and grief that can follow a traumatic birth, especially when a carefully prepared birth plan goes awry. With her permission, I’ve woven parts of her prenatal, birth, and postpartum journey into this post, highlighting her struggle with postpartum depression to honor her experience and offer recognition to others who may relate. My hope is that anyone reading this who has experienced challenges related to perinatal mental health may feel seen, less isolated, and better equipped with resources and support.
Consent Statement: This story is shared with full consent from Lauren, who hopes that by sharing her experience, others silently navigating birth trauma may find recognition, validation, and a sense of community. Her goal is to shed light on what often goes unspoken—and to help someone else feel less alone and more empowered.
Pregnancy and Birth: A Sudden Emergency
Lauren experienced gestational diabetes during her pregnancy. Even so, doctors can usually help manage this condition with careful monitoring and care. With good prenatal care, most people with this diagnosis have healthy pregnancies and deliveries.
Lauren followed medical advice, and her doctor reassured her that both she and her baby were doing well.
However, towards the end of her third trimester she developed a headache and brain fog. As time went on through the day, her vision blurred, and she started to feel scared. She called her doctor and was told to go to the hospital right away. Her husband was at work at the time, and rushed home when he got her call. Walking out of the house together was the last thing Lauren remembered before waking up in the hospital after an emergency c-section.
Lauren had a clear birth plan, but instead, she regained consciousness in a hospital room feeling alone, groggy, confused, and scared. Her husband and the medical staff told her that she’d had two eclamptic seizures: one on the pavement outside her home and another in the ambulance.
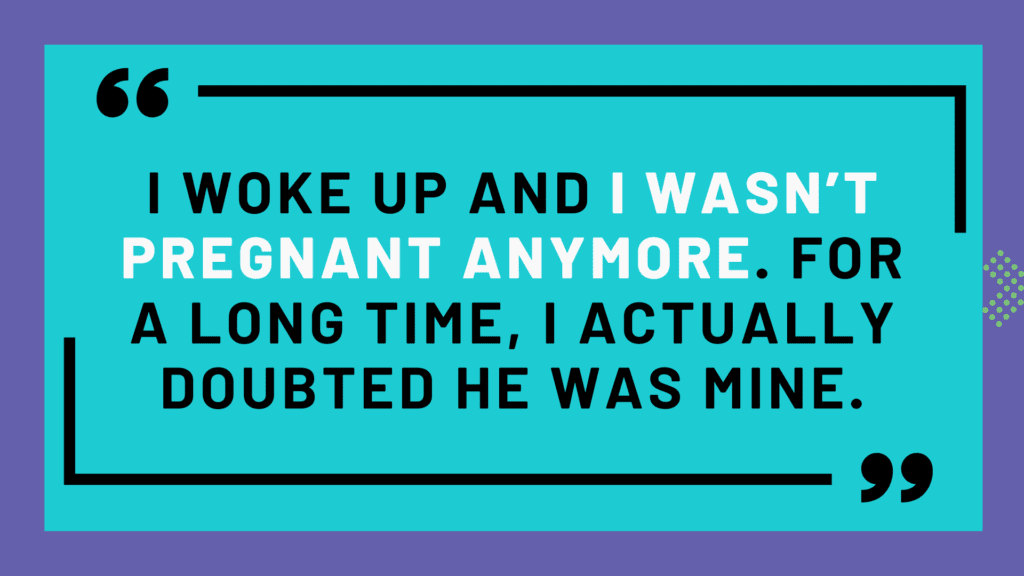
Now, she was disoriented, and had no memory of her son’s birth. Her husband was also in shock.
“There wasn’t a debriefing,” Lauren shared. “No one explained what had happened or gave us space to process it.”
During our interview, Lauren shared that she is now involved in advocacy efforts to improve the emotional and mental health support for people facing traumatic medical events and conditions such as postpartum depression.
“There wasn’t a social worker, or anyone with a mental health background to come talk to me.”
Part of her advocacy is to ensure that there are standard protocols in hospitals and medical settings for patients to discuss and process these types of experiences.
Postpartum Depression, Adjustments, and Challenges
Lauren was grateful to be alive, and that her baby was too. But she felt deeply disconnected from the birth, from her baby, and from herself as a new mother. She returned to work and even changed jobs, hoping a shift in environment might lift the weight. It didn’t.
“I would cry all the time,” she recalled. “I thought, what am I doing?”
Over time, the shame and disorientation built steadily throughout the first year. When she tried to share what she was going through, many people dismissed it. Instead of validating her pain, “You’re okay,” they said. “At least he’s healthy.”
Lauren was experiencing postpartum depression, a form of postpartum mood and anxiety disorder (PMAD). But at the time, she didn’t have a name for what she was feeling, just an overwhelming sense that something was wrong and no space to safely talk about it.
Emotional Impact
What she longed for was so simple: “Friends and family who came over, dropped off food, told me to lie down, and took care of the baby.” But this support was few and far between.
Lauren named this to identify a cultural gap in how we support new mothers, especially those recovering from traumatic births.
Societal expectations often place unrealistic pressure on new mothers to manage everything themselves, overlooking the vital role that practical and emotional support plays in healing. Tangible help like meals and childcare, combined with compassionate listening, can make a profound difference.
Unfortunately, work demands, social stigma, or discomfort talking about mental health often prevent families and communities from providing this essential care.
Lauren’s advocacy now focuses on closing this gap, promoting a culture that values and supports mothers during this vulnerable time.
Seeking Support
New mothers need mothering themselves with both tangible and emotional support. Simple acts of care.
“Listening alone is helpful,” she said. “People asked what happened, but I felt like it would take three hours to tell the story each time.”
What she needed were more frequent, low-pressure check-ins: ones that made space for how she was doing in the present moment.
Postpartum Adjustment
It took months for Lauren to feel bonded with her son.
“For a long time, I still felt pregnant,” she said. “Logically I knew I’d had a baby, but emotionally I hadn’t caught up. I’d touch my belly and think ‘where did he go?’”
The daily kicks were gone. In their place, a strange emptiness.
To help bridge the gap, she began writing to him.
“Not about my emotions, but about his life, from my lens. ‘We went to this person’s house, and you really liked this.’ I started collaging in the journal too. That helped me feel like I was part of his life, even when I didn’t feel like myself.”
“I didn’t live up to what everyone expected of me and to what I expected from my body. I felt like I was failing him [my husband], and like I was one failure away from falling apart completely.”
She had grown up caring for younger siblings and expected parenting to come naturally, especially to her. In her mind, it was her husband who might struggle with the transition. When her birth plan unraveled, followed by mastitis, postpartum depression, and a long recovery, the shame deepened.
Looking back, she recognizes how hard she was on herself.
“I had really high expectations. But no one told me any different. They had those expectations too.”
On top of everything, there was a national formula shortage.
“I just remember thinking, ‘can something go right? When is it going to ease up?”
Relationship and Emotional Health
Lauren’s husband was the only one who witnessed everything she went through. But that didn’t mean it was easy to talk about it together.
“Being honest with him was the scariest part,” she said. “It meant admitting how much I was struggling with intrusive thoughts, mood swings, anger, sadness. It felt like just another way I was failing.”
She feared that opening up would confirm what she worried about most: that she wasn’t cut out for motherhood.
“I thought I was supposed to be a superhero.”
Her husband was struggling too, especially given how different reality was from the original birth plan.
“It brought out the worst in both of us,” she said. “We were just trying to cope. But there was no roadmap. No one told us what trauma could do to you, as a couple, as parents, as people.”
Navigating the effects of postpartum depression placed further strain on their relationship, reinforcing the importance of communication and mutual support
Underlying Trauma
The birth experience also surfaced old, unresolved trauma for Lauren. “I didn’t want to give those memories airtime. They hurt,” she said. “But after 35 years of not dealing with them, the birth trauma cracked everything open. It all came flooding back.”
The emotional wave was overwhelming. “The hardest part was that I didn’t have the usual mechanisms to push things down anymore.”
The First Birthday After an Altered Birth Plan
As her son’s first birthday approached, Lauren began to feel it in her body. The milestone brought up physical reminders and emotional flashbacks.
“My emotional mind was terrified of seizures and of reliving the nightmare. A simple headache was enough to knock me off my feet.”
She had started therapy a few months earlier, in August, Lauren sought out a new provider—someone who specialized in postpartum mood and anxiety disorders (PMADs), birth trauma, and EMDR. She described this new therapeutic relationship as lifesaving.
Reflecting on that experience, Lauren shared, “It was the first time I didn’t feel ashamed.” She had the language for what I was going through.
Therapy gave Lauren space to name the intrusive thoughts she had been too afraid to say out loud. Beyond that, it gave her tools to process what had happened, and a path toward healing.
Reframing Her Body
One of the most transformative moments came early on.
“I remember looking at my stomach and my C-section scar, and I just held it.”
In therapy, Lauren began to challenge the expectations she had placed on her body—and those placed on it by society. She had believed, “My body didn’t do what it was supposed to do.” But in time, that belief began to shift. “It kept me alive,” she realized.
“I’m so protective now of my body.”
Groundwork and Coping Tools
Much of her therapy involved building emotional resources before diving into trauma processing. Visualization exercises helped Lauren regulate her emotions: moving from a distressing memory to a place of calm and safety. She practiced tuning into sensory details—such as what she could see, hear, smell, and feel—to reduce the power of traumatic memories.
Then, her therapist helped her break down overwhelming moments into smaller, manageable parts. “What did you feel in your body the moment you called your doctor?” As a result, the step-by-step unpacking made the memories less consuming.
EMDR added a visual element that Lauren found both engaging and grounding. During virtual sessions, she followed a moving ball across the screen as part of the bilateral stimulation. “I picked yellow,” she said. “It makes me feel like I’m bringing light into a dark space.”
Support and Resources That Helped
Lauren began writing down how she felt, either in a journal or in the Notes app on her phone.
“It helped me visualize the data—how many days I felt depressed, anxious, easily irritated, or distracted. Having that insight into myself was critical.”
Through my own research, I learned about the Preeclampsia Foundation and their amazing resources. “Knowledge is power,” she said. “Use the resources that feel right for you. There are so many out there.”
“I wasn’t showing up for myself for a very long time,” Lauren admitted. Therapy helped her begin to reclaim that self-care and self-worth.
In fact, her husband supported her emotionally and practically. When she shared her struggles with mood, anxiety, and intrusive thoughts, he listened.
“He saw it coming. When you’re in tune with your partner, you can usually tell something is going on, even if they’re not ready to acknowledge it themselves.”
Vulnerability was scary, but it created space for deeper connection.
He didn’t just say, “You should go to therapy.” He said, “You’re going to therapy, I’ll take care of childcare,” and he actually followed through. That was just as important as being emotionally available.
Medical and Perinatal Mental Health Care
Medication might help, and your doctor can help you decide what’s right for your body. Doctors most commonly prescribe antidepressants to treat depression. You can explore medication resources for lactation and pregnancy through the links provided here.
Evidence-based therapy types may include Cognitive Behavioral Therapy (CBT) and Interpersonal Psychotherapy (IPT), but others are also an option. A combined approach of medication and therapy is recommended for postpartum mood and anxiety disorders at the onset of symptoms. Postpartum Support International (PSI) provides specialized perinatal mental health resources through their HelpLine and Provider Directory.
Social and Emotional Support
This includes activities like prioritizing sleep, time for self, reading, podcasts, meditation, asking for help & support groups.
Active listening from family and friends is also key.
“I didn’t expect people to help me fix the trauma. Just listening is validating. It reduces isolation. It helped me feel like what I went through really was hard, and it doesn’t have to define me or my relationship with my son.”
Intentional bonding time was essential for Lauren.
“That time is so critical,” she said. “If I didn’t have paid leave, it probably would’ve taken me even longer to feel connected to him.”
Reflecting on her marriage, Lauren said, “For couples, try not to fall into rigid gender roles. This is a transformational time. Sometimes, you’re both just figuring it out. Tag-teaming. Giving grace. That’s what matters.”
Having access to a visiting nurse or similar support can make a major difference for new parents, especially those recovering from birth trauma.
Lauren experienced frustrating disconnects between her care providers, highlighting gaps in perinatal mental health care.
“I’d go to the nutrition class, then to my fetal medicine doctor, then to my OB[/GYN].”
But no one connected the dots. She believes medical providers need to communicate more—and consider the whole patient, including mental health.
Importantly, Lauren isn’t calling for every provider to be a mental health expert. But she is calling for more awareness. “They should recognize when someone might need extra support. They should ask. They should connect us to the right resources.”
To Those Who Are in It Now
If any part of Lauren’s story resonates with you—if you’re navigating trauma, pregnancy complications, a traumatic birth, or post partum anxiety and mood concerns, please know you are not alone, you matter, and connection and healing is possible.
And if you or someone you love is looking for emotional support, Council for Relationships offers therapy services for individuals, couples, and families navigating the transitions of pregnancy and parenting. Our therapists and psychiatrists in the Women’s Psychological Health Services are here to walk with you through these deeply human moments—with curiosity, compassion, and care.
If you’re looking for a way to honor your story or support others impacted by Preeclampsia and/or Eclampsia, consider joining the Promise Walk for Preeclampsia with the Philadelphia chapter of the Preeclampsia Foundation on, May 31, 2025 at the Navy Yard in South Philadelphia. It’s a chance to build community and raise awareness for families navigating the long-term impact of birth complications.
Editor’s Note: The views expressed in this blog are those of the author and do not necessarily reflect the official policy or position of Council for Relationships.
Therapy & Psychiatry at Council for Relationships
At Council for Relationships, we believe healing is possible for everyone, particularly when navigating the complexities of postpartum depression, disrupted birth plans, and perinatal mental health challenges. Our expert therapists and psychiatrists offer compassionate, specialized support tailored to your unique mental health journey.
Whether you’re seeking trauma-focused care, EMDR therapy, help recovering from postpartum depression, processing an altered birth plan, or addressing broader perinatal mental health needs, we’re here to help you find clarity and resilience.
About the Author
Amy Jones, MSW, MFT, LCSW, is the Director of Women’s Psychological Health Services and a Staff Therapist at Council for Relationships. Amy specializes in supporting women dealing with postpartum depression, disrupted birth plans, and broader perinatal mental health concerns. Her compassionate approach helps clients process trauma, anxiety, and identity transitions related to pregnancy, birth, and motherhood.
To begin your healing journey from postpartum depression, to process your birth plan experiences, or to address your perinatal mental health, request an appointment with Amy today.
About Women’s Psychological Health Services
Women’s Psychological Health Services (WPHS) at Council for Relationships provides expert, empathetic care specifically for women facing postpartum depression, birth plan disruptions, and perinatal mental health challenges. Our dedicated clinicians deliver personalized support, drawing from extensive training in evidence-based practices, including EMDR therapy, to effectively address the emotional impacts of pregnancy, birth trauma, and motherhood.
Whether you’re navigating postpartum depression, managing a changed birth plan, or exploring perinatal mental health resources, WPHS is ready to support you. Get matched with a WPHS therapist today.
More Mental Health Resources for Postpartum Depression and Recovery
Council for Relationships offers comprehensive mental health support with over 80 expert therapists and psychiatrists, including many skilled in EMDR therapy for trauma recovery and managing postpartum depression, birth plan challenges, and perinatal mental health needs.
Find the clinician who best meets your unique circumstances. Stay informed and supported by subscribing to our newsletter for mental health tips, expert resources, and important updates. To further explore topics like postpartum depression, birth plans, perinatal mental health, and more, visit our CFR blog.
Closing the Gap: Perinatal Mental Health Services in North Philadelphia
Emily Mudd: Celebrating the Founder of Council for Relationships | Part One
Emily Mudd: Celebrating the Founder of Council for Relationships | Part Two